What is Polycystic Ovarian Syndrome?
Polycystic Ovarian Syndrome (PCOS) occurs in approximately one in ten premenopausal women in Australia. It can develop in early adolescence but is usually diagnosed between late adolescence and menopause. Women with a family history of PCOS or type 2 diabetes may be more likely to develop this condition.
PCOS is diagnosed when a woman has two or more of the following three conditions:
• Increased levels of androgen hormones (which can also cause acne, excess body hair and loss of hair from the scalp)
• Irregular menstrual cycles
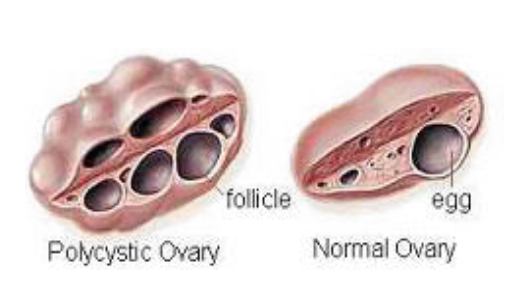
• The appearance of cysts in the ovaries (called polycystic ovaries) when incomplete ovulation occurs. These are viewed on an ultrasound.
Symptoms
Women with PCOS often experience one or more of the following symptoms:
Irregular menstrual periods
Fertility problems
Skin problems such as acne, dandruff and oily skin
Excess body hair
Difficulty losing weight.
What causes polycystic ovarian syndrome?
The exact cause of PCOS remains unclear, however it is suggested that genetics plays a role as women with PCOS are more likely to have a sister or a mother or who also has the syndrome. More recent research suggests that insulin resistance is a major underlying cause of PCOS, as 70-80% of women with PCOS have insulin resistance.
Insulin resistance
When foods containing carbohydrates are eaten the carbohydrate is converted to glucose and enters the blood stream. As the blood glucose levels (BGLs) rise a hormone called insulin is released. Insulin helps to carry the glucose into the body’s cells to be used as energy. The BGLs then return to normal levels.
In insulin resistance, the cells do not take up the glucose from the bloodstream as efficiently as they should. The body responds to this by producing more insulin to normalise BGLs. Increased insulin levels cause the ovaries and the adrenal glands to produce an enzyme that stimulates androgen production. Increased androgen production is one of the three key diagnostic criteria of PCOS.
How is PCOS treated?
Many clients can put PCOS into remission simply by following dietary and lifestyle advice. Others may require some medications or the contraceptive pill for assistance. Some other women may purely need to focus on reducing the symptoms of their PCOS. The following interventions are essential:
Weight loss
Weight loss is recommended for women with PCOS who are overweight or obese. Modest weight loss of 5-10% can significantly improve insulin resistance and assist with normalisation of menstrual cycles. Aim to avoid fad diets and make sustainable dietary and physical activity changes.
Carbohydrate intake
Having large portions of carbohydrate foods makes your pancreas work harder to produce more insulin, thus worsening insulin resistance. Avoid having large portions of carbohydrates. Your dietitian will teach you how much carbohydrate you need to meet your requirements, and how to distribute it throughout the day.
Choose low Glycaemic Index foods
Choosing foods with a low Glycaemic Index (GI) means that your body doesn’t have to produce as much insulin as quickly as the carbohydrates break down more slowly. This helps to improve insulin control. Look for foods with a lower glycaemic index.
Physical activity
Physical activity assists with weight loss and improves insulin resistance. Aim for at least 30 minutes of moderate-intensity physical activity on most days of the week. Increasing incidental activity, such as walking to the shops instead of driving or taking the stairs instead of the lift can be beneficial as well.
